Hepato-Biliary & Portal Interventions
What Are Hepato-Biliary & Portal Interventions?
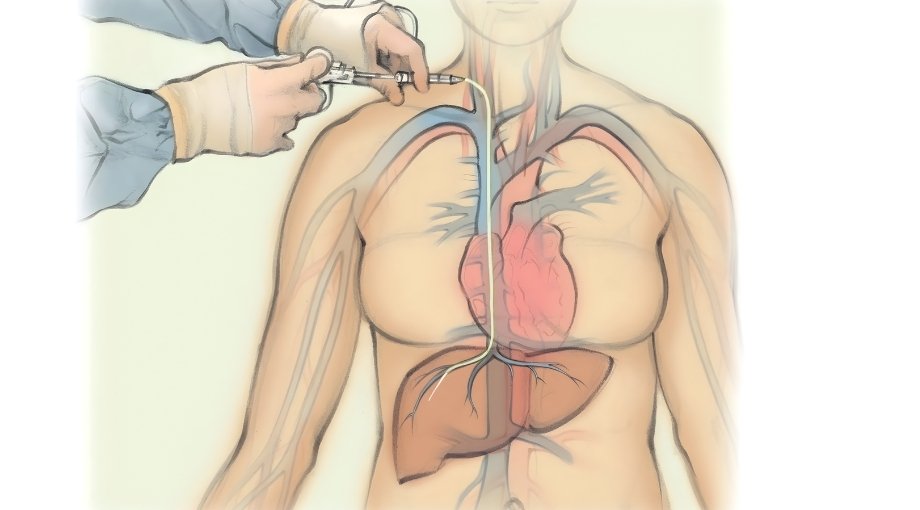
Hepato-Biliary & Portal Interventions are minimally invasive, catheter-based procedures performed under real-time imaging such as ultrasound, CT, or fluoroscopy.
These procedures are designed to diagnose and treat liver disease, portal hypertension, biliary obstruction, and complications related to liver dysfunction.
They help improve liver blood flow, relieve bile or portal vein obstruction, evaluate liver pressures, and enable safe liver tissue sampling. By avoiding open surgery, these interventions provide faster recovery, lower complication risk, and effective symptom control.
Symptoms of Hepato-Biliary & Portal Interventions?
Liver, biliary, and portal venous disorders can cause discomfort, jaundice, swelling, or gastrointestinal bleeding. Early identification and intervention prevent complications and improve quality of life.
Fluid accumulation in the abdomen due to liver disease or portal hypertension.
Blockage of bile ducts by stones, strictures, or tumors causing itching and liver dysfunction.
Variceal bleeding or portal hypertension-related hemorrhage.
Enlarged Spleen or Portal Vein
Symptoms like pain, hypersplenism, or portal vein obstruction.
Poor Liver Function
Signs of chronic liver disease including fatigue, confusion, or low platelet count.
Recurrent Biliary Obstruction
Obstruction causing repeated jaundice, cholangitis, or liver dysfunction.
Abdominal Swelling or Ascites
Fluid accumulation in the abdomen due to liver disease or portal hypertension.
Jaundice or Yellowing of Skin
Blockage of bile ducts by stones, strictures, or tumors causing itching and liver dysfunction.
Gastrointestinal Bleeding
Variceal bleeding or portal hypertension-related hemorrhage.
Poor Liver Function
Signs of chronic liver disease including fatigue, confusion, or low platelet count.
Enlarged Spleen or Portal Vein
Symptoms like pain, hypersplenism, or portal vein obstruction.
Recurrent Biliary Obstruction
Obstruction causing repeated jaundice, cholangitis, or liver dysfunction.
Aftercare & Lifestyle
Recommendations
Common Causes for Hepato-Biliary & Portal Interventions

Liver Cirrhosis or Fibrosis
Chronic liver disease leading to impaired portal circulation.
Portal Hypertension & Varices
Increased pressure in the portal vein causing gastrointestinal bleeding.
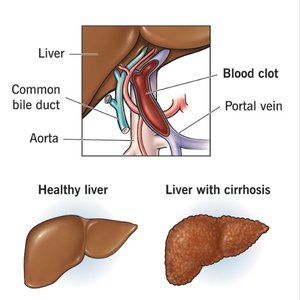
Portal Vein Stenosis
Reduced portal vein patency impairing liver perfusion.
Suspected Liver Lesions
Requiring image-guided liver biopsy for diagnosis.

Ascites Refractory to Medication
Persistent fluid accumulation requiring intervention.
Diagnostic Tests for Hepato-Biliary & Portal Interventions
Precise imaging is crucial for planning safe, effective interventions.
Ultrasound (USG)
Real-time guidance for biopsies, biliary drainage, and portal vein interventions.
CT Scan
Cross-sectional imaging to locate liver lesions, bile ducts, and vascular structures accurately.
Fluoroscopy
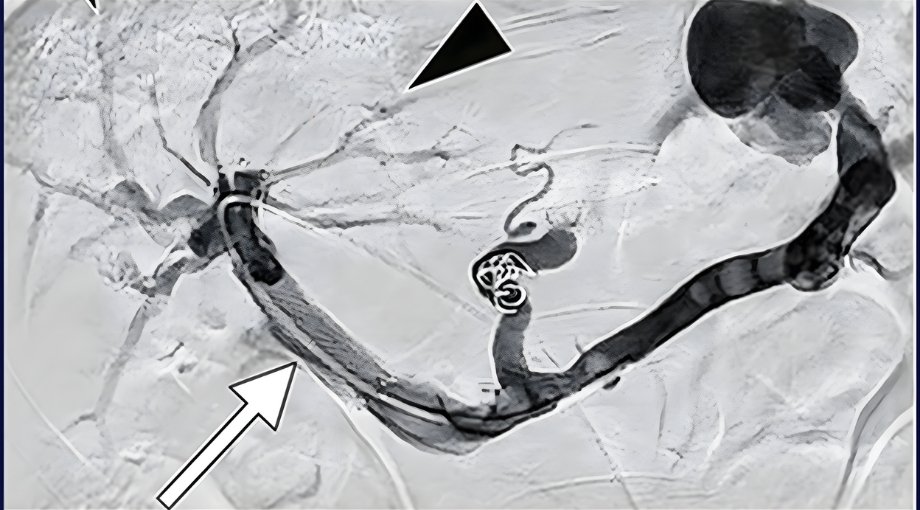
Live X-ray imaging used during TIPS, stent placement, or biliary interventions for precise guidance.
Portal Venography
Evaluates portal vein anatomy and pressure before stenting or shunt procedures.
Specialized Procedures Under HBP Interventions
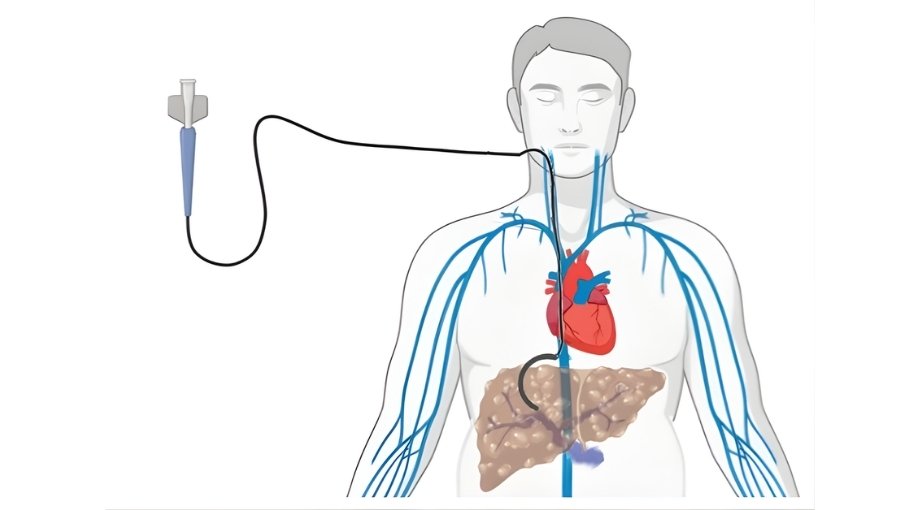
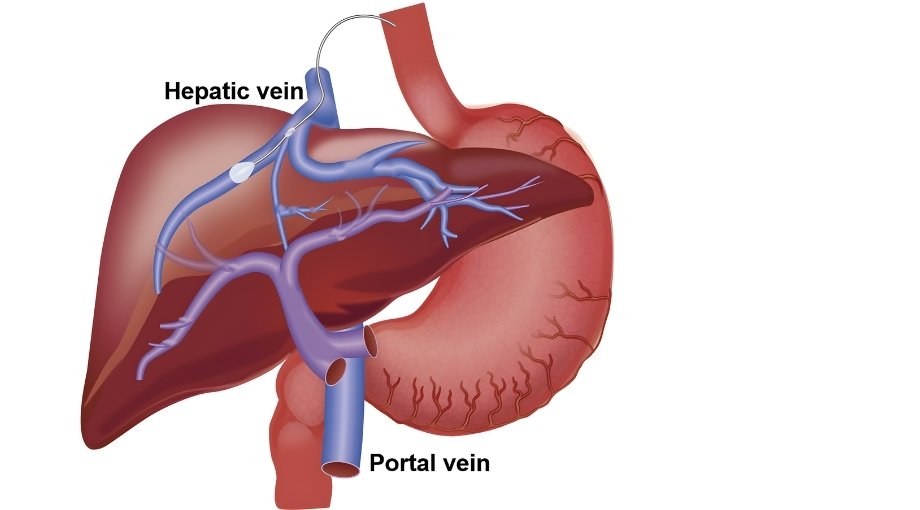
Transjugular Intrahepatic Portosystemic Shunt (TIPS)
TIPS is a minimally invasive procedure used to reduce high blood pressure within the portal vein system, commonly seen in patients with advanced liver disease. By creating a controlled channel between the portal vein and hepatic vein, TIPS helps redirect blood flow and reduces complications such as variceal bleeding and ascites. The procedure is performed under imaging guidance, offering effective symptom relief while avoiding major surgery.
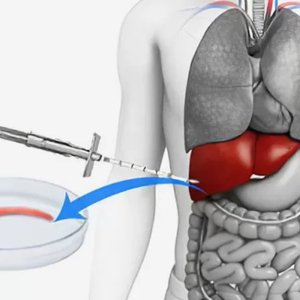
Transjugular Liver Biopsy
Transjugular liver biopsy is a safe alternative to conventional liver biopsy, especially in patients with bleeding risk, ascites, or advanced liver disease. The biopsy is performed through a vein in the neck, allowing liver tissue sampling without puncturing the liver capsule. This approach significantly reduces bleeding risk while providing accurate diagnostic information essential for liver disease evaluation and management.
HVPG Measurement (Hepatic Venous Pressure Gradient)
HVPG measurement is a specialized diagnostic procedure used to assess the severity of portal hypertension. By measuring pressure differences within the hepatic veins, this test helps determine disease progression, bleeding risk, and treatment effectiveness. HVPG plays a crucial role in guiding clinical decisions for patients with chronic liver disease and portal hypertension.
Portal Vein Stenting
Portal vein stenting is performed to restore blood flow in cases of portal vein narrowing or blockage due to thrombosis, tumors, or post-surgical changes. Using minimally invasive, image-guided techniques, a stent is placed to keep the vein open and improve circulation. This helps reduce portal hypertension-related complications and supports better liver function.
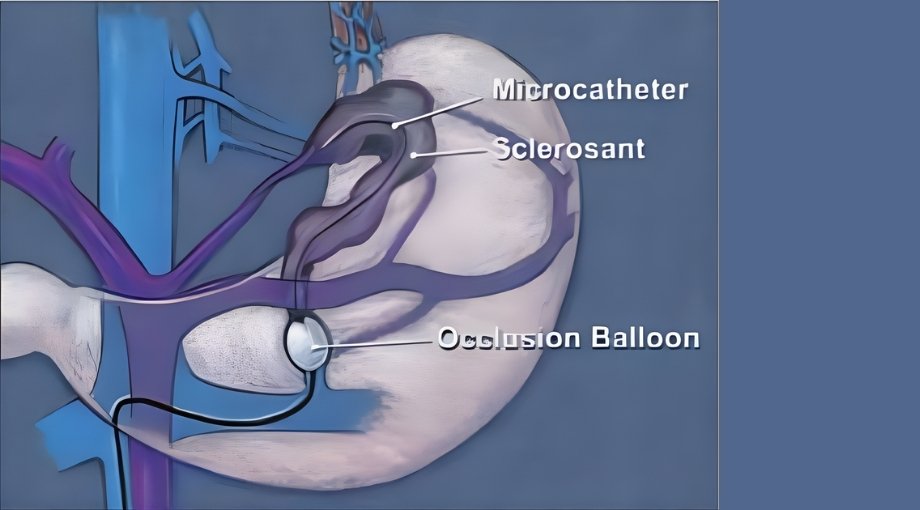
PRTO / BRTO
PRTO and BRTO are specialized procedures used to treat gastric or ectopic varices caused by portal hypertension. These techniques work by selectively blocking abnormal shunts and redirecting blood flow, reducing the risk of life-threatening bleeding. Performed under precise imaging guidance, PRTO/BRTO offer effective bleeding control while preserving liver circulation.
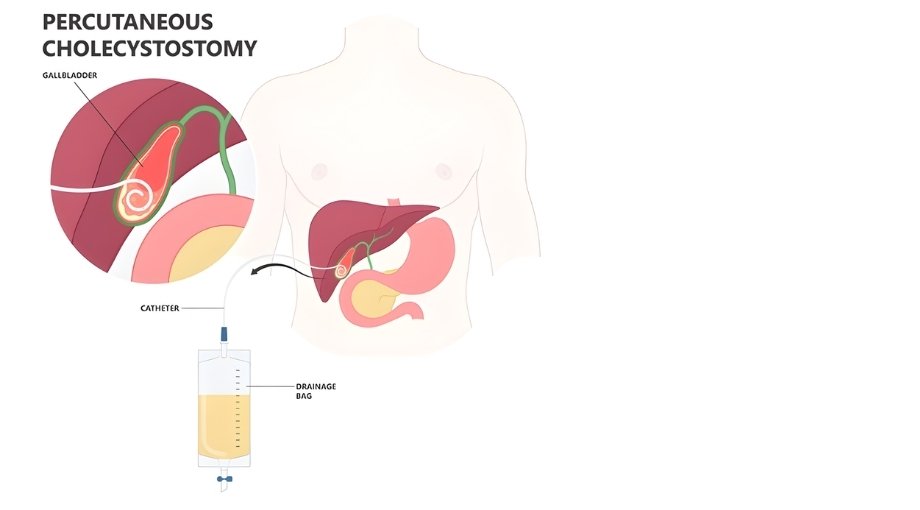
PTBD (Percutaneous Transhepatic Biliary Drainage)
PTBD is a minimally invasive procedure used to relieve bile duct obstruction caused by tumors, stones, or strictures. A drainage catheter is placed through the liver into the bile ducts to allow bile to drain externally or internally. This helps reduce jaundice, infection, and liver damage, while improving patient comfort and preparing for further treatment if required.
Benefits of
Minimally Invasive Hepato-Biliary & Portal Interventions
Treatments are done through tiny punctures with no large incisions.
Most patients resume daily activities within 1–2 days.
Procedures use local anesthesia and precise image guidance.
Less bleeding, minimal bruising, and reduced infection risk.
Maintain liver function while treating disease or complications.
Aftercare & Lifestyle Recommendations

Avoid heavy exertion initially

Maintain hydration and nutrition
Coordinate ongoing liver or oncology care

Follow-up imaging as advised

WHY CONSULT
Dr. Vatsal Agrawal?
01. Dual FVIR Fellowships
Advanced training from Nanavati Max Hospital and Mumbai Vascular Foundation (MVF).
02. Experience Across Major Hospitals
Worked with top centres including Hinduja, Saifee, Breach Candy, Nanavati Max, Raheja, and Heart & Vascular Superspeciality Hospitals.
03. Expertise in Liver & Portal Interventions
Skilled in TIPS, liver biopsy, HVPG measurement, portal stenting, PRTO/BRTO, and PTBD.
04. Patient-Focused Approach
Clear counselling, personalized planning, and dedicated follow-up ensure best long-term outcomes.
Frequently Asked Questions
No, local anesthesia and sedation ensure minimal discomfort.
Most patients return to normal activity within 1–2 days.
Yes, ideal for high-risk or elderly patients.
Yes, it effectively lowers portal pressure and prevents bleeding.
Transjugular approach minimizes bleeding risk and is very safe.
Most are day-care or short-stay procedures.
International Recognition & Approval
Percutaneous Biliary Drainage (PTBD)
Approved by the European Association for the Study of the Liver (EASL)

Transjugular Intrahepatic Porto-Systemic Shunt (TIPS) and Percutaneous Biliary Drainage (PTBD) are recommended by the European Association for the Study of the Liver (EASL) as safe and effective, minimally invasive procedures for managing portal hypertension and biliary obstruction, reducing complications, and improving liver function.

Dr. Vatsal Agrawal

He is a skilled Vascular & Interventional Radiologist known for performing advanced, minimally invasive arterial treatments with precision and safety.
Book Your Consultation With Dr. Vatsal
Get advanced, image-guided treatment for liver, biliary, and portal venous disorders with minimally invasive interventions.


